Tuberculosis (TB) of the musculoskeletal system, thought accounts for only 1-3 % of total TB cases 1 however, as n fourth of all TB cases are in India.
TB of the hip joint is comprised of 15% of all osteoarticular tuberculosis.
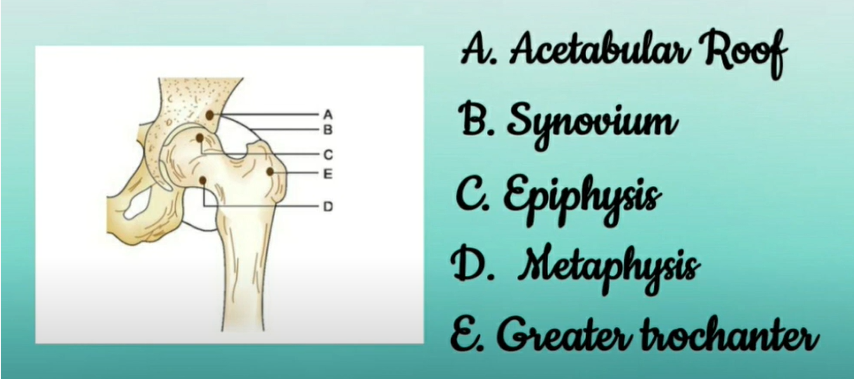
The area of infection that is majorly targeted is,
- Acetabular roof (A)
- Synovium (B)
- Epiphysis (C)
- Metaphysis (D)
- Greater trochanter (E)
Pathogenesis:
The synovial membrane is one of the most commonly affected. Here, the tubercle formation causes synovial hypertrophy resulting in pannus formation. This pannus destroys the articular cartilage resulting in the development of fibrous ankyloses of the hip.
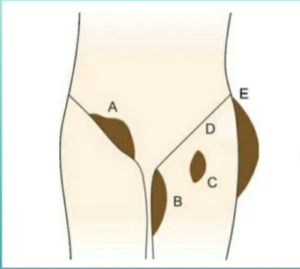
The smaller tubercles coalesce, undergo caseation, and form a cold abscess. This cold abscess tracks down along the areas of least resistance and may point in any one of the following sites.
- Inguinal region (A)
- Medial side of the thigh (B)
- Femoral triangle (C)
- Gluteal region (D)
- Lateral aspect of the thigh (E)
Clinical Features:
- Painful limp is the most common and early symptom.
- Antalgic gait with short stance phase.
- Pain becomes maximum at night.
- There may be wasting of the thigh and gluteal muscles.
- Tenderness may be elicited by direct pressure applied on specific points.
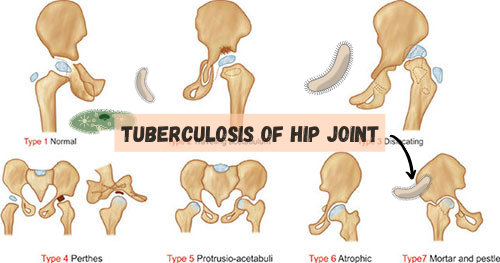
Stages of Tuberculosis (TB):
Stage 1: Stage of Synovitis
The disease is synovial with the patient assuming flexed, abducted, and externally rotated position of the limb. There is no real shortening and the extremes of movements are decreased and painful.
Stage 2: Stage of Early Arthritis
The local signs are exaggerated. The spasm/b s of the adductors and flexors results in flexion, adduction, and internal rotation of the affected limb. There is apparent shortening; significant muscle wasting and hip movement are decreased in all ways.
Stage 3: Stage of Advanced Arthritis
The flexion, adduction, internal rotation deformity found in Stage 2 are exaggerated. There is a true shortening with considerable restriction of hip movements and muscle wasting. There is gross destruction of the articular cartilage of the head of the femur.
Stage 4: Advanced Arthritis with Subluxation of Dislocation
Migrating acetabulum, frank pathological posterior dislocation, mortar and pestle hip, protrusio acetabuli are the features in this stage.
Deformities:
1. Flexion Deformity
In the initial stages of the disease, the patient keeps the hip in flexion, as this is the position of ease and of maximum joint capacity. Soft tissue contractures convert this into a fixed flexion deformity (FFD) making locomotion impossible. In an effort to bring the limb on the ground and make locomotion possible, the lumbar spine undergoes exaggerated lordosis and thus conceals the fixed flexion deformity.
2. Adduction Deformity
Soft tissue contractures convert the adduction position adopted by the patient due to the spasm of the adductor muscles following damage to the articular cartilage, to one of the fixed adduction deformities. The limb is now brought to the ground by the elevation of the pelvis as evidenced by the anterior superior iliac spine being at a higher level on the affected site. There is scoliosis of the spine away from the deformity.
3. Abduction Deformity
In the initial phases of the disease, because of the increase in the joint space due to effusion, the limb assumes a position of flexion, abduction, and external rotation. If fixed in this position by soft tissue contractures, the patient develops deformity. This limb is then brought to the ground by the downward tilt of the pelvis as evidenced by an anterior superior iliac spine (ASIS) lying at a lower level with the corresponding scoliosis of the spine towards the affected side.
4. Limb Length Discrepancy
In the initial stages, there may be apparent lengthening; but in the advanced stages, the patient develops shortening.
Preoperative Rehabilitation
- Helps to develop a patient-specific rehabilitation program to follow post-operative, taking assessment findings into consideration.
- Benefits: decreased length of stay, decreased anxiety levels, improved self-confidence, establish a relationship of trust between the therapist and patient.
Postoperative Rehabilitation
- Address the functional needs of the patient (e.g. start mobilizing) and improve mobility, strength, flexibility, and reduce pain. This starts off as an assisted process, but the aim is to get the patient as functional as possible.
- As a result of the underlying pre-operative pathology, patients may present with muscle atrophy and loss of strength, particularly in the gluteus medius and quadriceps muscles.
- Accelerated rehabilitation programs and early mobilization have been shown to give patients more confidence in their post-operative mobilization and activities of daily living, as well as being more comfortable with earlier discharge.
For more information talk to a healthcare provider.
If you have any questions about Tuberculosis of the Hip, please feel free and leave a comment.
Do share this blog with your friends and family!