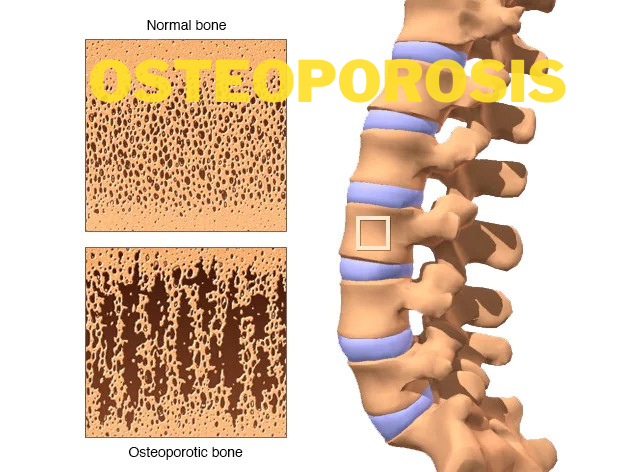
Osteo refers to bones and porosis means pores. So, osteoporosis is when there’s a higher breakdown of bone. A decrease in bone density to the point of potential fracture.
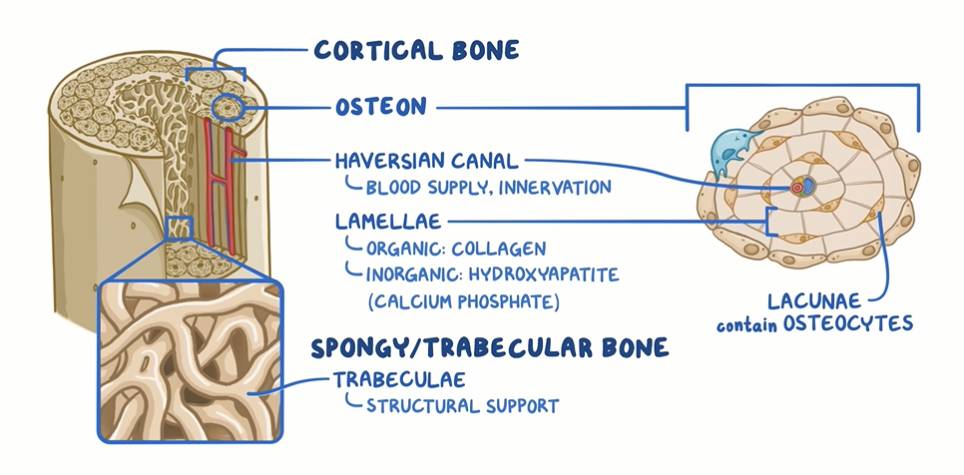
Looking at a cross-section of a bone, there’s a hard-external layer known as the cortical bone and a softer internal layer of spongy bone that is composed of trabeculae. The trabeculae are like a framework of beams that give structural support to the spongy bone. The cortical bone, in turn, is made up of many functional, pipe-like units called osteons, which run through the length of the bone.
In the center of these osteons, there are hollow spaces called Haversian canals, which contain the blood supply and innervation for the bone cells. Around the Haversian canals, there are concentric lamellae, which look a bit like tree rings.
The lamellae have an organic part, which is mostly collagen, and an inorganic part called hydroxyapatite, which is mostly calcium phosphate. In between neighboring lamellae, there are spaces called lacunae, which contain bone cells called osteocytes.
At first glance, the bone may appear motionless and unchanging, but it’s actually a very dynamic tissue.
Bone Remodeling:
In fact,
- Spongy bone is replaced every 3 to 4 years.
- Compact bone is replaced every 10 years.
In a process called bone remodeling which has two steps:
- Bone resorption: when specialized cells called osteoclasts break down bone.
- Bone formation: which is when another type of cells called osteoblasts form new bone.
Bone remodeling as a whole is highly dependent on serum calcium levels, which, in turn, are kept in the normal range by a balance between parathyroid hormone (PTH), Calcitonin, and Vitamin D.
Parathyroid hormone is produced by the parathyroid glands in response to low serum calcium, and it increases bone resorption to release calcium into the bloodstream.
On the other hand, calcitonin is produced by the thyroid gland in the response to high serum calcium, so it opposes the action of PTH- therefore promoting bone formation and decreasing bone resorption.
Finally, vitamin D promotes calcium absorption in the gut, so it increases serum calcium, promoting bone formation and decreasing bone resorption.
Peak Bone Mass
The balance between their regulatory factors results in a peak bone mass, usually by age 20 to 29 and this usually occurs earlier in females than in males. Factors that determine the peak bone mass are genetics. For example, people of African descent tend to have greater bone mass and nutrition.
Finally, strength training increases peak bone mass, as well as hormones like estrogens and androgens that inhibit bone resorption.
When osteoclasts break down bone faster than the osteoblasts can rebuild, it results in the lowering of the bone mass and eventually in osteoporosis.
Causes
Spongy bone and cortical bone, these bone changes increase the risk of fracture, and they are known as fragility or pathologic fractures. Some bones like the vertebrae, shoulder blades, and ribs consist mainly of spongy bone, so they are at great risk of fragility fractures.
Factors that accelerate bone mass loss and increase the risk of osteoporosis are low estrogen levels, like after menopause, and low serum calcium.
Additional factors include alcohol consumption, smoking, drugs that decrease calcium absorption from the gut through antagonism of vitamin D, and drugs like heparin and L-thyroxine.
Another factor is physical inactivity, as seen in astronauts in a zero-gravity environment where they just don’t use their musculoskeletal system as hard as when they’re on earth. As a result, bone deposition decreases due to a lack of stress, while resorption increases.
There are also diseases that can cause osteoporosis like
- Turner syndrome
- Hyperprolactinemia
- Klinefelter syndrome
- Cushing syndrome
- Diabetes mellitus.
Now, the two most common types of osteoporosis are
1. Postmenopausal osteoporosis
In postmenopausal osteoporosis, decreased estrogen levels lead to increased bone resorption.
2. Senile osteoporosis
People with senile osteoporosis don’t usually have symptoms until a fracture occurs.
Symptoms
The most common type of fractures are vertebral fractures, also known as compression fractures, and it occurs when one or more bones in the spine weaken and shatter. Vertebral fractures cause back pain, height loss, and a hunched posture.
Femoral neck fractures and distal radius fractures can also occur, and they’re often associated with postmenopausal osteoporosis.
Diagnosis
Osteoporosis is usually diagnosed with a dual-energy X-ray absorptiometry or DEXA scan which tests for bone density.
Treatment
Treatment for osteoporosis usually relies on bisphosphonate drugs like Alendronate and Risedronate. If osteoporosis is really advanced, teriparatide, a recombinant parathyroid hormone can be used.
We recommend you to take your doctor’s advice for proper guidance.
Do share this blog with your friends and family!